Cardiovascular Inflammation
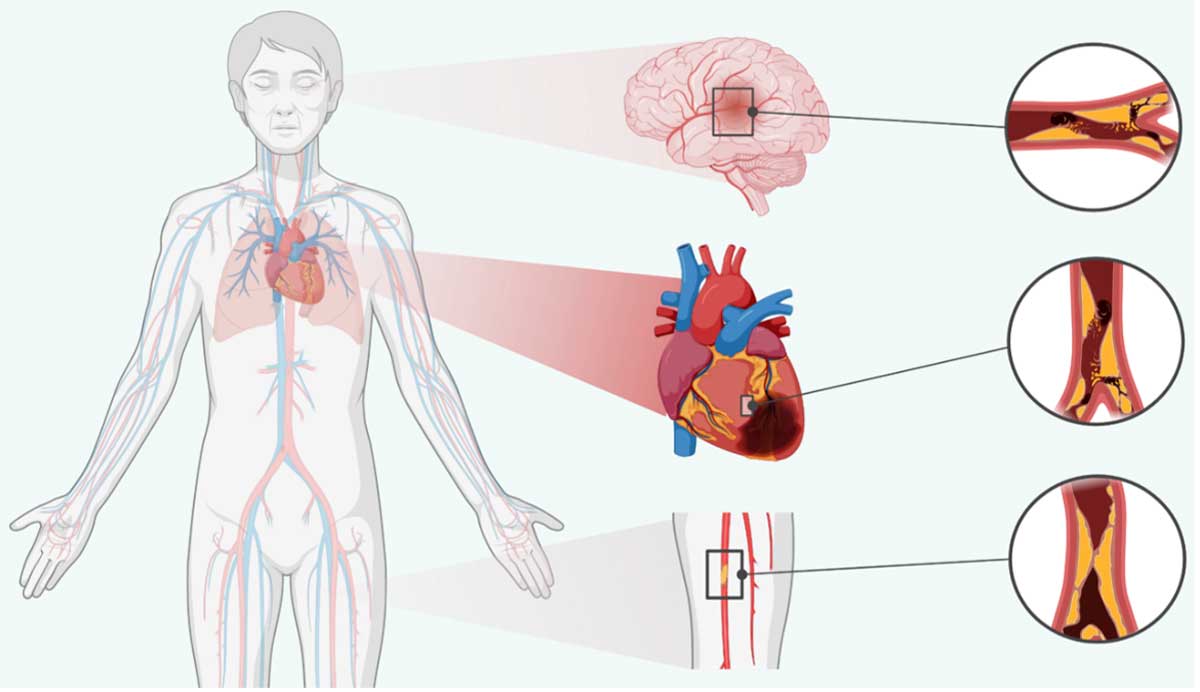
Cardiovascular disease (“CVD”) is a group of disorders that affect the heart and blood vessels and includes coronary artery disease, peripheral artery disease, stroke, heart failure, and abdominal aortic aneurysm. CVD is the leading cause of morbidity and mortality worldwide, with an estimated 20 million cardiovascular-related deaths in 2021. CVD-related deaths continue to increase each year despite the wide availability of targeted treatment options, indicating that current therapies are not adequately addressing all risk factors as the global population continues to grow and age.
Atherosclerotic Cardiovascular Disease (ASCVD)
Atherosclerotic cardiovascular disease (ASCVD) is a group of disorders caused by plaque buildup and rupture in the artery walls and includes myocardial infarctions (heart attacks), peripheral artery disease, and strokes. Despite the wide availability of once-daily, oral medicines including lipid-lowering therapies, antihypertensives, and antiplatelet agents, cardiovascular disease continues to be a leading cause of morbidity and mortality worldwide, with an estimated 20 million deaths per year. Given this high disease burden, we believe there is a significant unmet need for additional therapies that target alternative risk factors for ASCVD, particularly inflammation.
Role of IL-6 in ASCVD
The role of inflammation and IL-6 in ASCVD pathogenesis has been the focus of study for over two decades. Mechanistic studies have implicated IL-6 in plaque formation, erosion, and rupture as well as the formation of blood clots. Multiple clinical and human genetic studies have implicated elevated IL-6 signaling with risk of future major adverse cardiovascular events.
Biological processes contributing to ASCVD pathogenesis
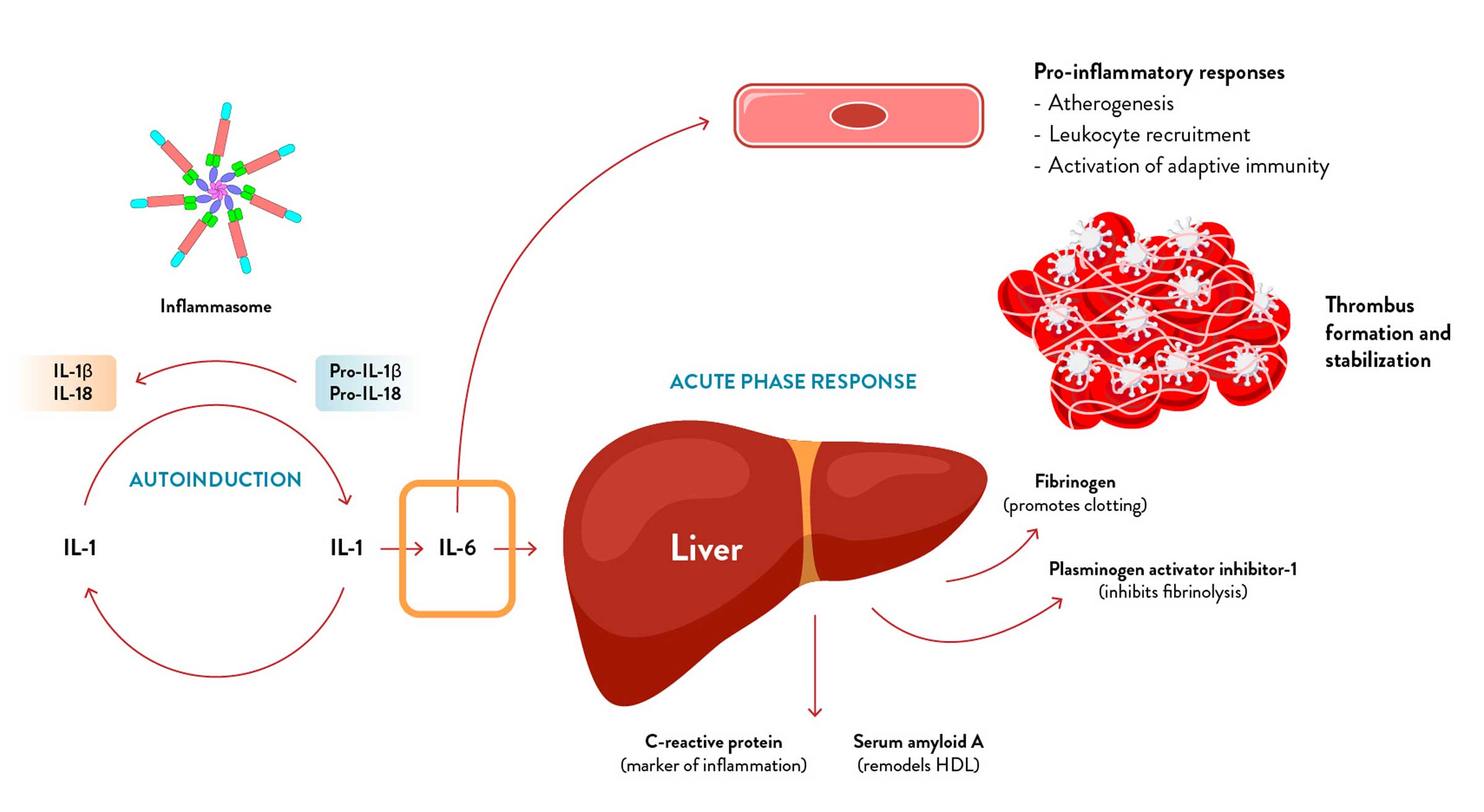
Adapted from: Libby et al., Cells (2021) and Libby et al., Int J Cardiol (2018)
Emerging breakthrough insights from the IL-6 renaissance have generated a wealth of evidence for the key role of IL-6 in ASCVD. Analysis of trial data across tens of thousands of ASCVD patients has demonstrated inflammation is a stronger predictor of risk of MACE and CV-related death than cholesterol levels. Studies of anti-inflammatory mechanisms in ASCVD have demonstrated the importance of specifically targeting IL-6 driven inflammation.
In particular, results from the CANTOS study showed that canakinumab, a monoclonal antibody which inhibits IL-1β, a key cytokine in the IL-6 pathway, significantly reduced MACE and CV death risk in ASCVD patients. Importantly, this benefit was notably larger in patients whose IL-6 levels were lowest following treatment with canakinumab.
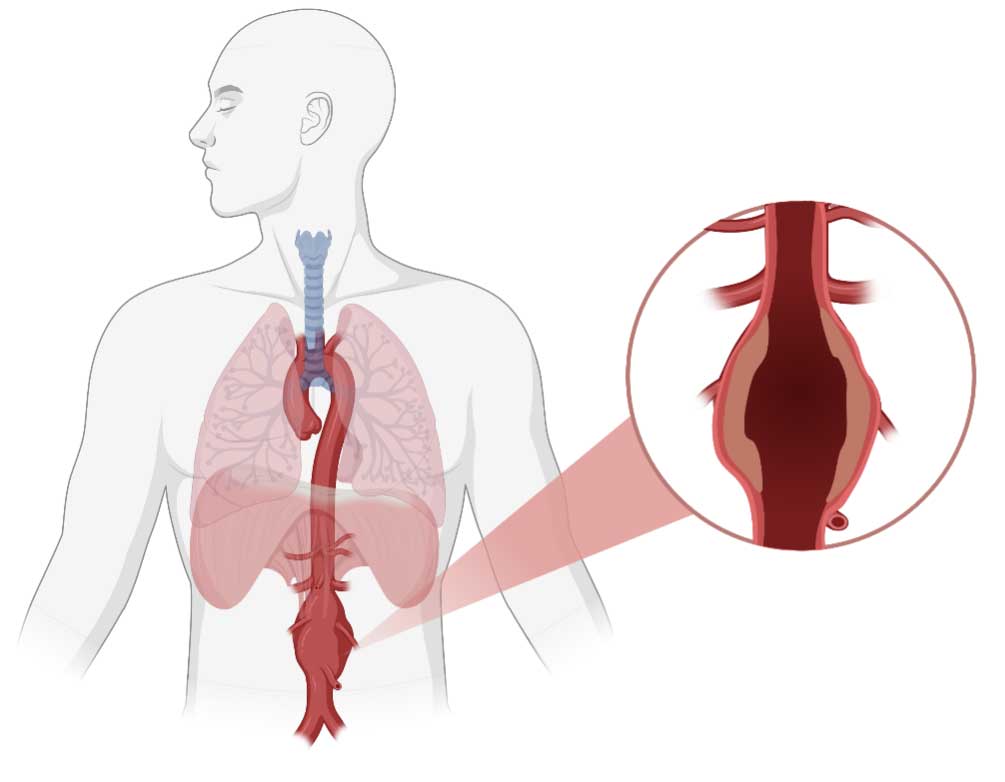
Abdominal Aortic Aneurysm (AAA)
Affecting approximately 2 million patients in the United States, AAA is a serious condition with high unmet need characterized by weakening and enlargement of the aorta, the largest blood vessel in the body. AAA is a focal expansion of the abdominal aorta usually diagnosed by a maximum aortic diameter of ≥30 mm on imaging (e.g., ultrasound). It is primarily associated with the degeneration of the aortic wall, leading to abnormal dilation and the potentially fatal rupture of the abdominal aorta. Surgical repair is the only currently available therapeutic option, and is indicated for patients who have experienced an aneurysm rupture or are at increased risk of rupture or have symptoms or other potential complications of AAA. Currently, there are no FDA-approved medical treatments for AAA, leaving patients with small and asymptomatic aneurysms no alternative but to be monitored until the threshold for surgery is met.
Role of IL-6 in AAA
The totality of data provide compelling evidence to support the therapeutic potential of IL-6 inhibition to slow AAA growth. Naturally occurring human genetic variants that mimic low-dose IL-6 pathway inhibition have been associated with statistically significant reductions in the risk of developing abdominal aortic aneurysm. Epidemiological evidence is supportive as well. Higher circulating levels of IL-6 and higher aortic tissue levels of IL-6 have been associated with the presence of abdominal aortic aneurysm. In addition, higher levels of hs-CRP have been associated with a higher risk of AAA and increased AAA size. Finally, experimental evidence has been supportive of the potential therapeutic impact of IL-6 inhibition on AAA. In mouse models of AAA, genetic and pharmacological inhibition of IL-6 pathway signaling have been associated with decreased aneurysm expansion.
Thyroid Eye Disease (TED)
TED, also known as Graves’ ophthalmopathy, is a debilitating autoimmune disorder that affects the eyes and surrounding tissues. It is commonly associated with Graves’ disease, an autoimmune disorder that affects the thyroid gland. The annual incidence of TED in the United States is estimated to be around 16 per 100,000 females and 3 per 100,000 males, or approximately 30,000 new cases a year.
TED occurs in two phases – the initial active phase, characterized by high inflammation which lasts between 6-36 months and the later inactive phase with lower inflammatory involvement. TED is characterized by the production of autoantibodies against thyroid-stimulating hormone receptor (TSHR) which are also implicated in Graves’ disease. These autoantibodies target the tissue surrounding the eye, leading to inflammation, swelling, and tissue remodeling.
TED can cause significant discomfort and can be sight-threatening if left untreated. Initial symptoms of TED may include dryness and irritation of the eyes, sensitivity to light, excessive tearing, double vision (diplopia), and a sensation of pressure behind the eyes. As the disease progresses, patients may develop retraction of their upper eyelids, swelling and redness around the eyes, and bulging of the eyes (proptosis). In severe cases, swelling and stiffness of the muscles that move the eyes can cause misalignment and even vision loss.
Role of IL-6 in TED
IL-6 is believed to play a critical role in the pathogenesis of TED, including in autoantibody production, T-cell mediated inflammation, and orbital fibroblast activity.
IL-6 INHIBITION HAS POTENTIAL TO BLOCK MULTIPLE STEPS IN TED PATHOGENESIS
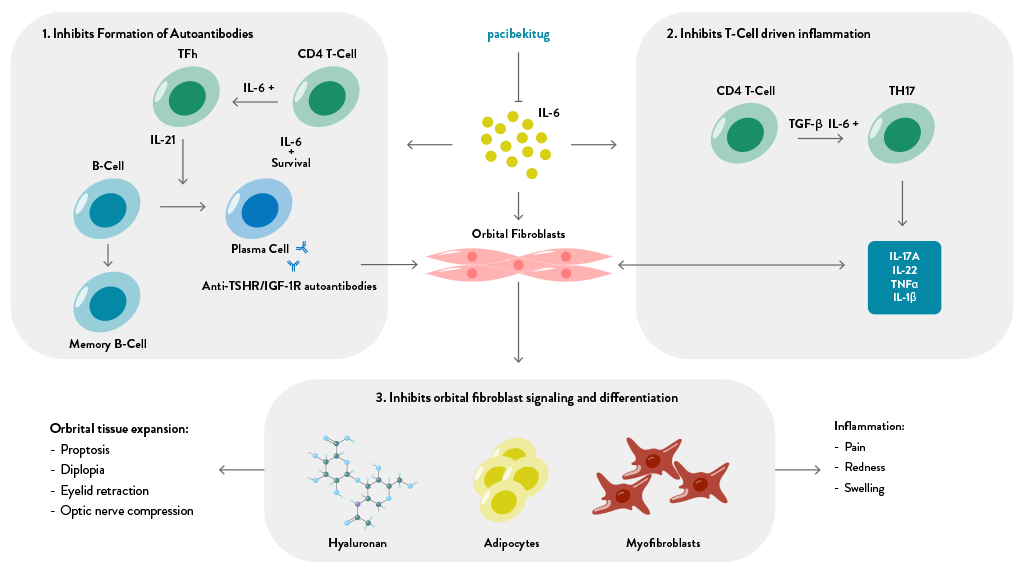
Adapted from: Huang et al., Eye (2018); Hodgson and Rajaii, Ophthalmol Ther (2020); Fang et al, Front Endocrinol (2021);
Smith et al., Eye (2019); and Cabezas et al., Front. Immunol. (2022)
There is a large body of evidence supporting the role of IL-6 in TED including:
- IL-6 and soluble IL-6R levels are elevated in TED patients and correlate with disease activity.
- In a study of Graves’ Disease patients, those that developed TED had significantly higher IL-6 levels than those that did not.
- A growing body of literature documents successful clinical experiences with other IL-6 pathway inhibitors, reporting meaningful improvements in proptosis, inflammation (measured by the Clinical Activity Score), and diplopia